Santa Claus Disease
Portraits of people with blackheads and red noses appear in seventeenth-century paintings. Artists of the past captured, for posterity, sufferers in the last stages of rosacea, known as rhinophyma, a common disease that affects the skin of the face. Since then, medicine has changed dramatically. Patients with inflamed skin are no longer subjected to bloodletting or leeching. Today's specialists offer their patients a much wider range of options and procedures to combat the ailment.
Cuperose or rosacea?
Beauty industry professionals are sometimes confused about the terms “couperose” and “rosacea.” While some consider couperose to be a disease in its own right, others believe that both terms refer to the same condition at different stages of development. Let's see who's right.
There is no diagnosis of couperose in the International Classification of Diseases. The term in medical circles refers to a condition in which a healthy capillary dilates and becomes visible to the naked eye. The word “couperose” was first coined by the French physician Guy de Chauliac in the 14th century. Dermatologist Thomas Bateman, in 1812, gave these pathologically dilated vessels another name — “rosacea.” Since then, the terms “couperose” and “telangiectasia” have been used synonymously as “dilated capillaries,” while “rosacea” is a diagnosis of a chronic skin disease, the first stage of which is characterized by couperose.
The calling card of rosacea
Rosaceous acne and spider veins occur exclusively on the face. They can be localized, affecting only the nose, cheeks, or chin, or can affect several sites at once: chin and cheeks, nose and cheeks. Rosacea begins with congestion in the capillaries of the upper layers of the skin. As blood circulation slows down, the vascular walls are put under more strain, lose their elasticity, and become brittle.
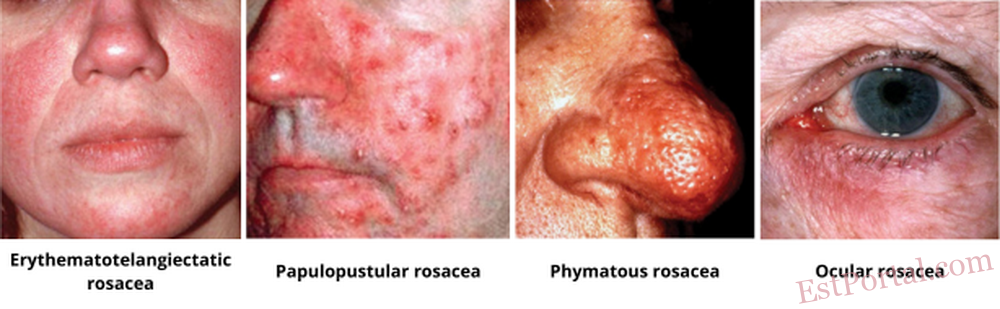
Visually, the first stage is quite modest: just a reddening of the skin, which becomes overly sensitive, with accompanying sensations of itching and burning. Over time, irritation and swelling become an integral part of rosacea patients' experience. Afterwards, individual capillaries appear in the form of stars or nets (telangiectasia).
In stage II, the reddened skin thickens, and papules or pustules with saprophytic or opportunistic microflora appear as shown by bacteriological cultures. The number of dilated capillaries increases. If the skin is not treated at this point, rosacea may cause more extensive damage later on: in its last stage, rhinophyma, nodules and sebaceous hyperplasia form, causing the skin to swell and become deformed due to persistent swelling and inflammation.
Another indispensable attribute of rosacea is a moist face. The reason is that under the influence of high pressure, some of the fluid from the lymph and vessels is released into the surrounding tissues. Some of the exuded moisture remains in the skin, causing swelling and hyperemia, and some of it finds its way into the epidermis and appears on the surface of the skin. This gives the impression of a permanently sweaty face. The sweat glands have nothing to do with it, though.
Whose fault is it?
The causes of couperose and rosacea are still unclear. Undoubtedly, there is a connection between skin problems and digestive diseases. The second undisputed fact is that rosacea occurs more often in patients with arterial hypertension: under the influence of high pressure, the blood vessels dilate, appearing on the surface as single dilated capillaries or vascular meshes. The latest findings suggest that the subcutaneous Demodex mite may not be the cause of the disease as previously thought, but it may well accelerate its progression. A subcutaneous inhabitant is detected in 90 percent of rosacea patients. The severity of the disease doubles if the mite is present. The reason why Demodex inhabits the affected skin is simple: the parasites are attracted by the moisture evaporating from diseased blood vessels and the swelling due to this process. Heredity plays a role in the development of the disease: if both parents suffer from rosacea, the risk of the disease in the child is 60%.
Provocative factors
Rosacea may be exacerbated by any action that causes vasodilatation and leads to stasis in the capillary network of the skin.
Sudden changes in temperature. Rosacea is known as the disease of cooks who spend most of their time at the stove. The disease thrives under the influence of temperature fluctuations, triggering persistent vasodilation. The same effect is seen in patients partial to saunas and baths.
Hot food and drinks. When hot food enters the digestive system, not only the digestive tract organs become hot, but also the face. Hot tea or soup causes the blood vessels to dilate.
Alcoholic drinks. Alcohol dilates blood vessels. This applies not only to cognac, but also to wine, especially red wine. Although the mechanism of this drink's effect on rosacea is not fully understood, you can say with certainty that the disease is more severe in red wine drinkers.
Stress. In case of nervous overload, the large main vessels constrict and the blood pressure rises, while the peripheral vessels in the capillary network, on the contrary, expand.
Ultraviolet light. The sun is a serious trigger for rosacea. It produces a thermal effect and simultaneously affects the skin with ultraviolet light. Intense insolation during an acute flare-up period may cause exacerbation of nearly all symptoms. Only after a course of treatment does the sun become safe, and the tan will mask the skin blemishes.
Rosacea and age
It's a fact that most rosacea patients are in their third decade. A younger body can more easily cope with the triggering factors. However, dilated capillaries should not be thought of as the prerogative of the elderly alone. It is not uncommon for 16-year-olds to be affected by the disease. An interesting correlation can be noticed: if a person has their first hypertensive crisis in their teens, rosacea is likely to make itself felt by the age of 40.
5 steps in the treatment of rosacea
For any form of rosacea, whether couperose or rhinophyma, the patient is prescribed a standard treatment regimen: first, the triggering factor must be removed, then the dilated capillaries must be treated, internal and external treatments must be prescribed, and proper home care must be provided. Let's look at each stage of treatment.
No. 1: Addressing risk factors
If your patient has arterial hypertension, you need to stabilise their blood pressure. Of course, it is impossible to cure hypertension, but there are many ways to keep it under control. If a hypodermic mite has been detected, you will have to deal with it as well. Since hot food and drinks, as well as spicy food, contribute to blood rushing to the face, advise the patient to avoid or minimise their consumption. Brightly coloured foods are also undesirable for rosacea patients. Avoid drinking alcoholic beverages. You may have to give up going to the sauna and even change jobs if they involve fluctuating temperatures. In rosacea, you should not subject your body to strenuous physical activity. Exercising at the gym, for example, causes blood to rush to the head, which is dangerous for the blood vessels.
No. 2: Capillary removal
If a single dilated capillary appears on the face, it is impossible to shrink it back to its normal state. The only way to get rid of the cosmetic defect is to remove it.
How do you remove enlarged capillaries?
Electrocoagulation and laser removal are the most popular removal methods today.
The first method is considered somewhat outdated in aesthetic medicine clinics, but it has a strong list of arguments in its defense. Firstly, the coagulator blades are quite tiny, which means that they can be used to remove the smallest capillaries. Secondly, the electrocoagulator works point by point without involving neighboring skin areas. An indisputable advantage of working with the electric device is that the specialist controls the knife with his hand, which cannot be said for the laser beam. However, it takes several hours per patient.
The laser is considerably faster than the coagulator in terms of speed, but it is more traumatic because large areas of skin are affected during the procedure. The smallest attachment for a laser is 4 cm².
The mechanism of the coagulator is quite primitive: a thin needle (electric knife) is inserted into a dilated capillary, and a current is passed through it. The discharge heats the capillary up to 100°C, the protein folds, and a clot appears in its place, blocking the flow of blood. The result is visible to the naked eye instantly – a white spot appears on the skin. A coagulator is used to create several miniature blood clots in the blood vessel, so that after two weeks, the capillary has completely atrophied.
The laser acts in a similar way to the coagulator, only instead of small clots, one massive clot is formed.
No. 3: Strengthening blood vessels
After capillaries have been removed, prophylactic treatment is necessary. In order to prevent new capillaries from expanding, medication in the form of tablets, drops, or injections is needed to strengthen the vascular wall. The most commonly used products are ascorbic acid-based, a combination of ascorbic acid and rutin (vitamin P), and ginkgo biloba. Depending on the severity of the disease, the treatment course lasts from 1 to 3 months. It is advisable to repeat this therapy at least once a year.
No. 4: External remedies and salon treatments
Creams, masks, toners, and cleansing gels should be adapted to the skin of rosacea patients. Skin with capillary problems is particularly sensitive and prone to irritation, swelling, and inflammation. Therefore, cosmetic products containing skin irritants such as alcohol and acids must never be used. When planning the clinical treatment of couperose, it is necessary to select the procedure so as to affect each symptom separately. For example, microcurrent therapy, cryotherapy, and draining manual massages can help reduce inflammation and swelling.
In addition to its draining effect, microcurrent therapy stimulates the development of new cells in the vascular wall and therefore further strengthens the capillaries.
Cryotherapy uses machines with attachments in the form of irons, which help to cool the surface of the skin. The cold narrows the capillaries, relieving inflammation and swelling.
Chemical peels for rosacea
Peeling during an exacerbation can either improve or worsen the situation drastically. It all depends on how well you approach the procedure. Firstly, peeling is the removal of the keratinized layer of the epidermis, and secondly, the stimulation of the division of new skin cells by the irritant action of the acid.
The new layer of cells that appears after the peeling closes any damaged capillaries and improves the appearance of the skin. But only if the peeling has not damaged any inflamed or irritated skin areas. If the peeling doctor uses too high a dose of acid or the exposure time is incorrect, the patient will get a burn, and on already damaged skin. Mistakes during peeling can lead not only to a worsening of the appearance of the skin but can also prevent further treatment. Due to the constant secretion of fluid from the injured vessels, the burned surface will not heal well and will be festering. This will prevent the specialist from treating the dilated capillaries with a coagulator. The current will pass through the “wet” capillary, and the chemical burn will be joined by a thermal burn. It is safer to perform chemical peels during a remission period when intensive treatment has been completed. In this case, the new cell layers will hide traces of dilated capillaries and eliminate redness.
Which peels are suitable for rosacea patients?
During an exacerbation, it is best to use superficial peels with glycolic (oxyacetic) acid – this substance is the most tested, detailed, and predictable of all AHA acids. Interestingly, light enzyme peels are not suitable for rosacea, as they exfoliate more but stimulate much less the formation of new skin cells. During the remission period, the patient is prescribed median peels.
No. 5: Home care
Proper home care for rosacea is the key to rapid skin recovery. The client will need cleansing and toning products, as well as day and night creams. All products should be as mild and sparing as possible: alcohol-free, with minimal oil content. Alcohol irritates already irritated skin, and oils form a film and raise the temperature of the skin by several degrees. For skin with couperose, it is better to use water- or gel-based products.
In very severe rosacea (hypertrophic skin areas, deformed nose or cheeks), surgery must be performed.
“An Old Man and his Grandson” by Domenico Ghirlandaio
Rosacea is a chronic dermatosis that cannot be conclusively cured. But if the patient follows all the recommendations, you can safely guarantee near-perfectly clear skin. Otherwise, sooner or later, they may suffer the fate of the people depicted in 17th-century paintings.
Evgeniy EROSHKIN — MD, Doctor of Medical Sciences, Dermatovenereologist (Ukraine)