Многомерная оценка и хирургические подходы к омоложению шеи
Старение шеи является до сих пор актуальной проблемой, несмотря на то что за последние годы было описано множество техник и процедур коррекции этой зоны.1–8 Результат такой коррекции, выглядящий хорошо в раннем послеоперационном периоде, может сопровождаться в течение нескольких недель или месяцев раздражающей индурацией, дряблостью кожи, неровностями контура, возникающими из-за птоза слюнной железы, гипертрофии двубрюшной мышцы или подплатизменного жира, которым не занимались в течение основного хирургического вмешательства.
Несмотря на то, что большое количество хирургов настаивает на связывании платизмы, это решение проблемы не всегда приемлемо для пациентов с тонкой шеей. Далеко не все шеи похожи.
Старение шеи зависит от следующих факторов:
- возраст;
- эластичность кожи;
- количество аккумулированного поверхностного и глубинного жира в области шеи;
- качество и объём поддержки нижней челюсти;
- природная высота шейного отдела позвоночника;
- наличие артритных изменений шейного отдела позвоночника, влияющих на его высоту и вогнутость;
- индекс массы тела (ИМТ).
На старение шеи существенно влияют приобретённые или врождённые анатомические, эстетические и метаболические факторы. Старение этой зоны при низком индексе массы тела и длинной тонкой шее будет существенно отличаться от такового у пациента с высоким индексом массы тела, короткой шеей и слабой скелетальной опорой нижней челюсти. Между этими двумя крайностями есть огромное разнообразие различных случаев, требующих индивидуального подхода для адекватного лечения пациента.
В первом случае (низкий ИМТ, длинная тонкая шея с нормальным изгибом и достаточной опорой нижней челюсти) хорошо сработают простые техники — такие как шейно-лицевая подтяжка с бокового подхода. Во втором случае (высокий ИМТ, короткая шея, слабая скелетальная опора) эта простая процедура, которую рекомендуют многие хирурги, в лучшем случае даст посредственный результат, а в худшем случае — сделает более выраженными анатомические проблемы и связанные с ними эстетические деформации.
Этот простой анализ объясняет, почему нельзя использовать одни и те же техники коррекции для различных анатомических и клинических случаев.
Ожирение
Ожирение — это постоянно возрастающая проблема в большей части индустриализированного мира. Только в США насчитывается более 6 миллионов взрослых людей, страдающих ожирением. Также актуальна эта проблема среди детей и подростков. С 1980 года количество людей с избыточным весом выросло вдвое среди детей и втрое среди взрослых (по данным на 2006 год). Это люди, которых пластические хирурги будут рассматривать как пациентов, когда они достигнут среднего или пожилого возраста. И это не говоря о тех, кто уже достиг среднего и пожилого возраста. Ожирение влияет не только на туловище, но и на значительную часть лица и шеи. У таких пациентов подкожный жир накапливается не только в передней области шеи, но и в задней. У них он также накапливается глубоко на платизменной мышце, в отличие от людей со средним весом. Люди с избыточным весом, как и люди с ожирением, также имеют проблему с толстыми щеками и двойным подбородком. Ожирение является обязательным условием для рассмотрения при планировании операции.
Выступающая двубрюшная мышца
Выступающая передняя часть двубрюшной мышцы ещё одна проблема, на которую надо обязательно обратить внимание при проведении цервикопластики. Причиной этого выступания может быть гипертрофия или мальпозиция мышцы. Мне неизвестно, от чего наступает гипертрофия.
Мальпозиция передней части двубрюшной мышцы возникает вследствие низкой позиции подъязычной кости. Это видно по пациентам с тупоугольными и твёрдыми шеями, а также по пациентам с микрогенией.
Птоз слюнной железы
Птоз слюнной железы является ещё одной комплексной проблемой. Он наблюдается у многих пациентов и усложняет процесс создания нормального контура шеи во время цервикопластики. Птоз слюнной железы может наблюдаться у пациентов с тонкими или тяжёлыми шеями. Предоперативно эту проблему легче выявить у пациентов с тонкими шеями. У пациентов с тяжёлыми шеями начальная и даже значительная степень птоза слюнной железы бывает скрытой. Это может стать ловушкой для неопытного хирурга потому, что если вы пропустите это, в результате будете иметь недовольного пациента: он заявит, что вы не удалили ему этот кусочек жировой ткани, что очевидно не так. Помочь таким пациентам будет нелегко, и коррекция на этой стадии проходит значительно тяжелее.
Дегенерация шейного отдела позвоночника
Постепенное сокращение шейного отдела позвоночника вследствие артритных изменений или естественного сжатия, или грыжи межпозвоночных дисков. Обычно эти явления не отмечены в этиологии эстетических проблем шеи в процессе её старения.
Такие изменения являются обычными для позвоночника по всей длине, и для шейного отдела они не являются исключением. Эти изменения укоротят шейный цилиндр, который в свою очередь вытолкнет глубинную шею и нижнюю часть ротовой структуры в зону наименьшего сопротивления, каковой является треугольник под нижней челюстью и между шеей и подбородком. Как следствие, слюнная железа, двубрюшная мышца и подплатизменный жир образуют грыжу спереди и сзади. Более поверхностный шейный конверт, кожа и платизменная мышца станут тоже более избыточными как в горизонтальном, так и вертикальном измерениях.
Скелетальная опора нижней челюсти
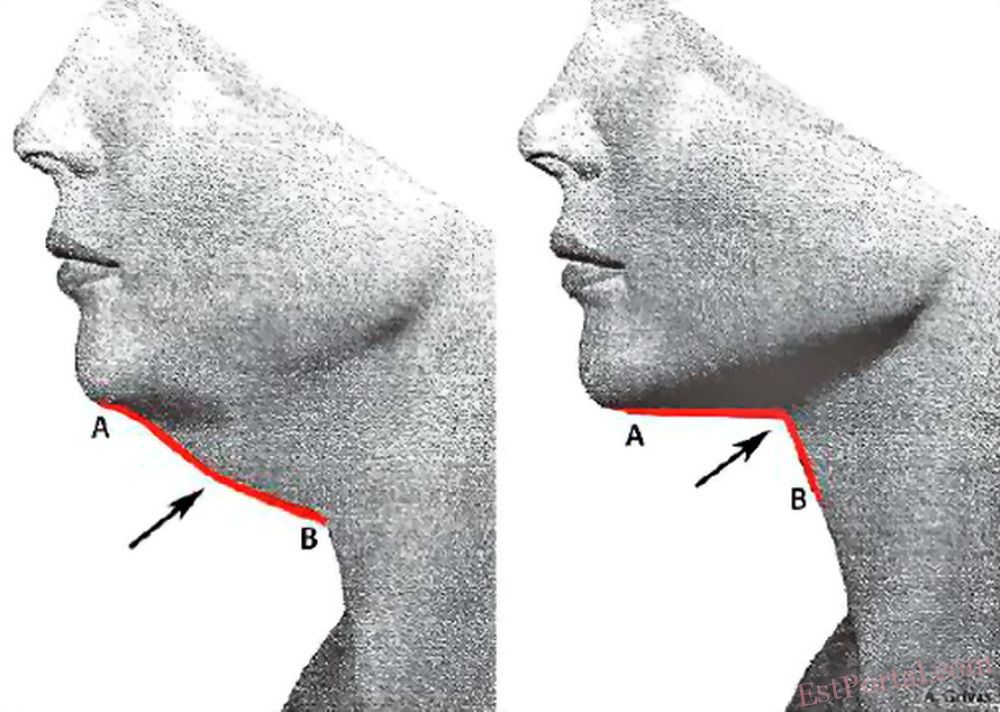
Размер скелетальной опоры нижней челюсти также влияет на процесс старения нижней части лица и шеи. Плохая опора на подбородке, тело нижней челюсти и угол влияют на смещение структур нижней части лица в сторону шеи, притупляя впадину под нижней челюстью и меняя цервикоментальный угол на более тупой. Это также приведёт к более заметному выступанию подчелюстных структур.
Предоперационное планирование
Подробный и обязательный анализ является важным для хорошего хирургического планирования. Пациента необходимо проконсультировать по всем вопросам, описанным в обзоре: описать количество поверхностного и глубинного шейного жира, качество скелетальной опоры вокруг подбородка и нижней челюсти; объяснить, насколько толстым или тонким является шейный цилиндр, какие структуры выступают, присутствует ли птоз слюнной железы; оценить количество избыточной кожи, наличие или отсутствие тяжей платизмы и тому подобное.
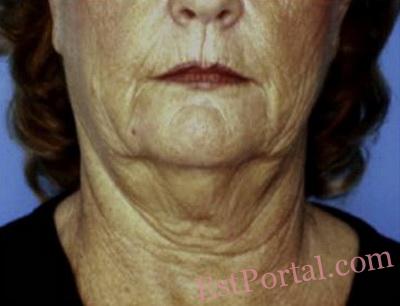
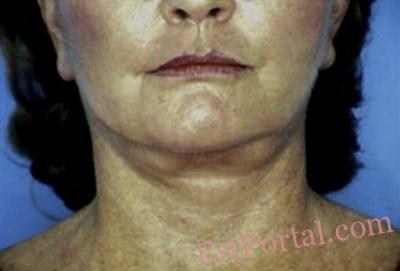
Основываясь на этих выводах, хирург делает предложение. Вам необходимо подчеркнуть необходимость увеличения скелетальной опоры и обсудить лечения глубинных шейных структур, особенности подхода к коррекции шеи. Вы используете боковой подход или ещё дополнительно примените передний? Как вы будете лечить платизму и кожу? Это важные решения, так как цервикопластика не даст хорошего результата без надлежащей скелетальной опоры. Если у пациента тяжёлые глубокие структуры, то результатом стандартной цервикопластики постоперационно может стать тяжёлая шея. Поскольку лечение птоза слюнной железы является самым тяжёлым и длительным, пациенты должны хорошо понимать процесс и последствия подхода. Очень часто пациенты принимают решение исходя из экономических факторов. Он или она должны понимать, что после проведения операции могут быть остаточные эффекты, в том числе заметные проблемы, такие как выступание слюнной железы, которую не заметили в процессе операции (Рис. 1 и Рис. 2).
Рис. 1. Эту пациентку записали на двухплоскостное лицевое омоложение в связи с полнотой глубинной шеи, связанной с птозом и увеличением слюнной железы. Она решила не лечить птоз слюнной железы.
Рис. 2. Постоперационно, несмотря на улучшение на другом уровне, она демонстрирует акцентированную полноту слюнной железы.
Когда вы добавляете более сложные процедуры к стандартной шейно-лицевой подтяжке, это увеличивает время операции и её стоимость. Это отчасти оправдано, если вы добавляете увеличение подбородка и угла нижней челюсти, а также глубокую цервикопластику. Во многих случаях компоненты запланированных операций должны выполняться поэтапно для достижения наилучшего результата и предотвращения длительного нахождения пациента под анестезией. Стандартная предоперационная оценка сердечно-сосудистого риска, предотвращение разжижения крови, контроль повышенного кровяного давления проводится у всех пациентов.
Обязательно проводится послеоперационное наблюдение пациента под контролем сертифицированной медсестры с опытом работы в пластической хирургии.
Время выздоровления пациента и возвращения к работе зависит от продолжительности хирургического вмешательства. Оно может колебаться от 1 до 4 недель.
Хирургическая техника
Боковой и передний подходы
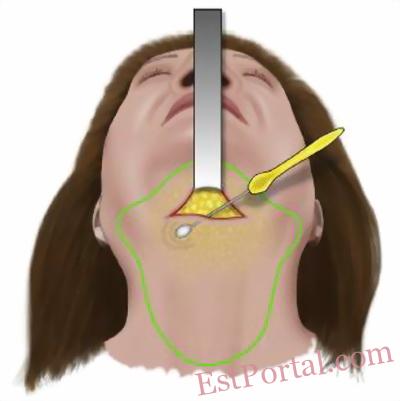
У большинства пациентов применяются боковой и передний разрезы. Этот подход хорош вне зависимости от возраста пациента и количества работы, которую следует провести. Причиной того что многие пациенты нуждаются в проведении работ на их передней части шеи, становятся платизма, субментальный жир и т. п. Я получил наилучший контроль над этими структурами благодаря субментальному разрезу. Субментальный разрез обычно делают на 1,0-1,5 см позади складки на подбородке. Это позволяет мне провести подкожную диссекцию из этого разреза к передней нижней части подбородка и отделить соединение кожи со складкой под подбородком и перед челюстными соединениями.
Такая диссекция сопровождается кровотечением, и я могу контролировать это подкожное кровотечение наилучшим образом при использовании этого подхода. Данная диссекция позволяет лучше редрапировать кожу. Этот надрез под подбородком также позволяет поднять платизму посередине и переместить кожу в противоположном направлении. Обычно это невозможно сделать при использовании только бокового подхода.
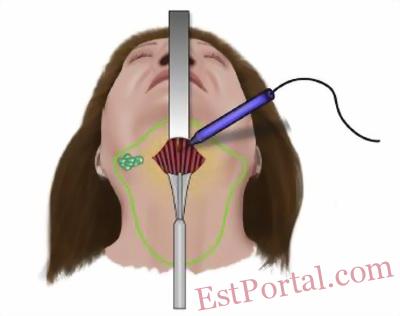
Рис. 3. Надрез под подбородком при использовании переднего подхода выполняется на 1,0-1,5 см позади складки под подбородком.
Рис. 4. Широкий подкожный разрез проведён с помощью субментального подхода. Как минимум 0,5 см подкожного жира должно быть сохранено.
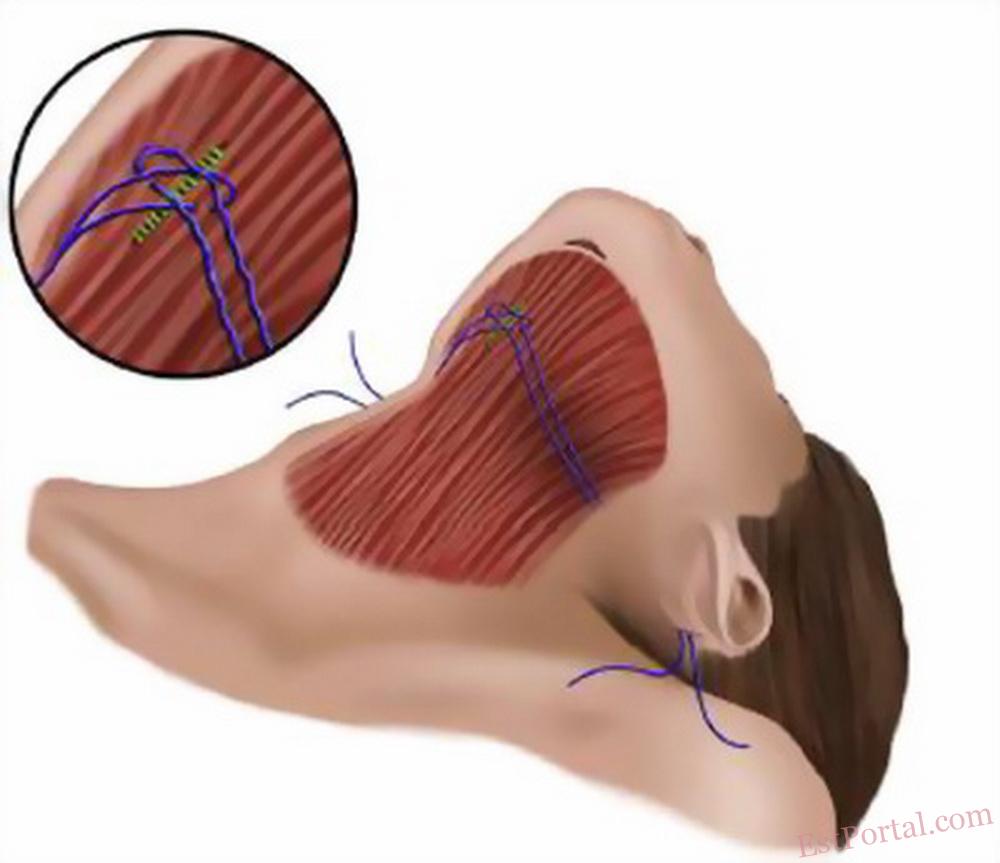
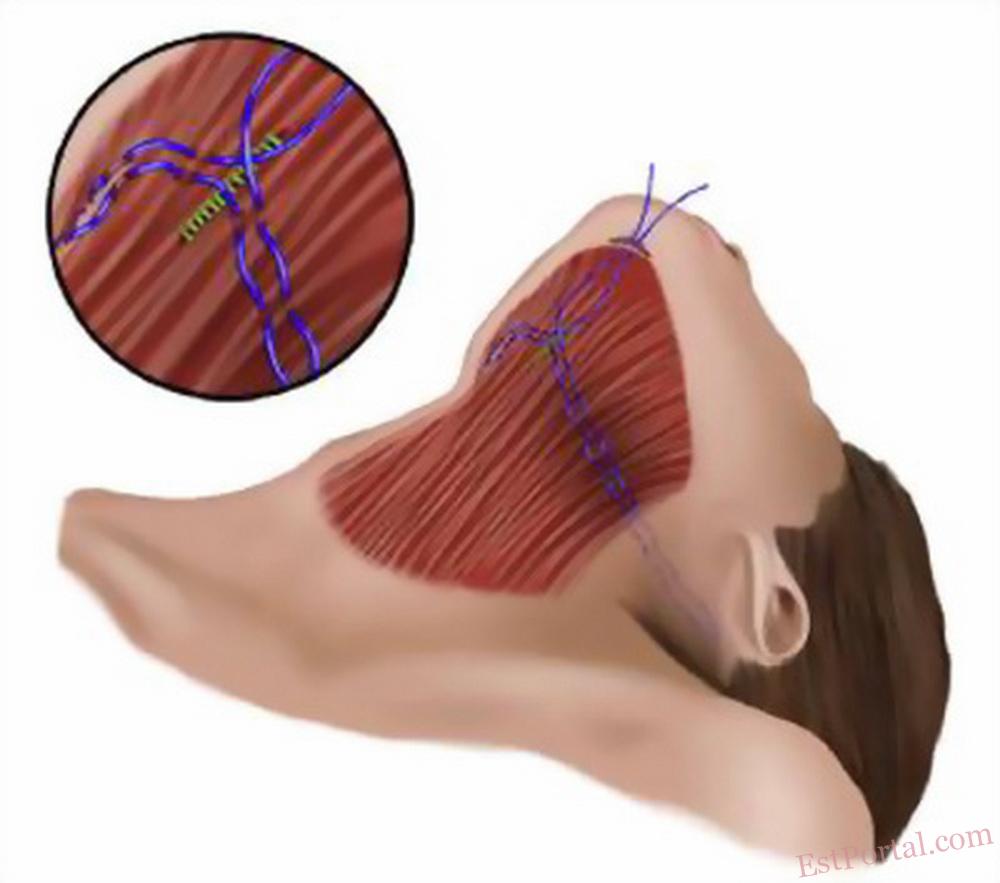
Рис. 5. Изображено поднятие замкнутого шейного шва Giampapa.
Боковой подход
Очевидно, что существуют исключения, когда нет необходимости проводить эти манёвры, и вы можете справиться со всем, используя боковой подход.
Сам по себе боковой подход назначается в случае, когда имеется:
- гладкая зона складки под подбородком;
- отсутствие выпуклости подбородка;
- отсутствие тяжей платизмы;
- отсутствие видимых предчелюстных ямочек.
Рис. 6. The Ramirez Pursestring шов. Это вариация GSS. Двойной ряд швов проходит сквозь платизму. Этот манёвр привлекает мышцы над слюнной железой для дополнительной поддержки при работе с избытком платизмы.
С другой стороны, я использую надрез под подбородком только с молодыми пациентами или у пациентов среднего возраста, так как у них не такой значительный избыток кожи, и большинство проблем находятся в зоне подбородка (Рис. 3 и Рис. 4). Остальные проблемы шеи могут быть откорректированы путём липосакции и шовной подтяжки через заушный/мастоидный мини-надрез, как описано у Giampapa и DiBernardo (Рис. 5).9 Если есть избыток кожи, то он может быть редрапирован в направлении назад с помощью разреза кожи, используя мини-надрезы в заушной/затылочной зоне и применяя модификацию шовной подтяжки Giampapa Рамирез (Рис. 6).
Для этого необходим эндоскоп, что позволит провести точную диссекцию и контролировать кровотечение.10 Ментопексия и/или имплантаты подбородка также требуют переднего надреза.
Шейный жир и шейные выпуклости
Удаление жира с шеи проводится путём прямой очистки ножницами через субментальний подход. Я использую липосакцию только когда применяю полностью закрытый подход или уменьшение объёма тяжёлых подкожных отложений жира, а далее делаю хорошие контуры ножницами.
Решение о резекции жира под двубрюшной мышцей или под мышцей платизмы принимается во время операции.
Рис. 7. Подходя к глубинному отделу шеи, платизма открывается вертикально от передней точки выступания подбородка до уровня перстневидного хряща.
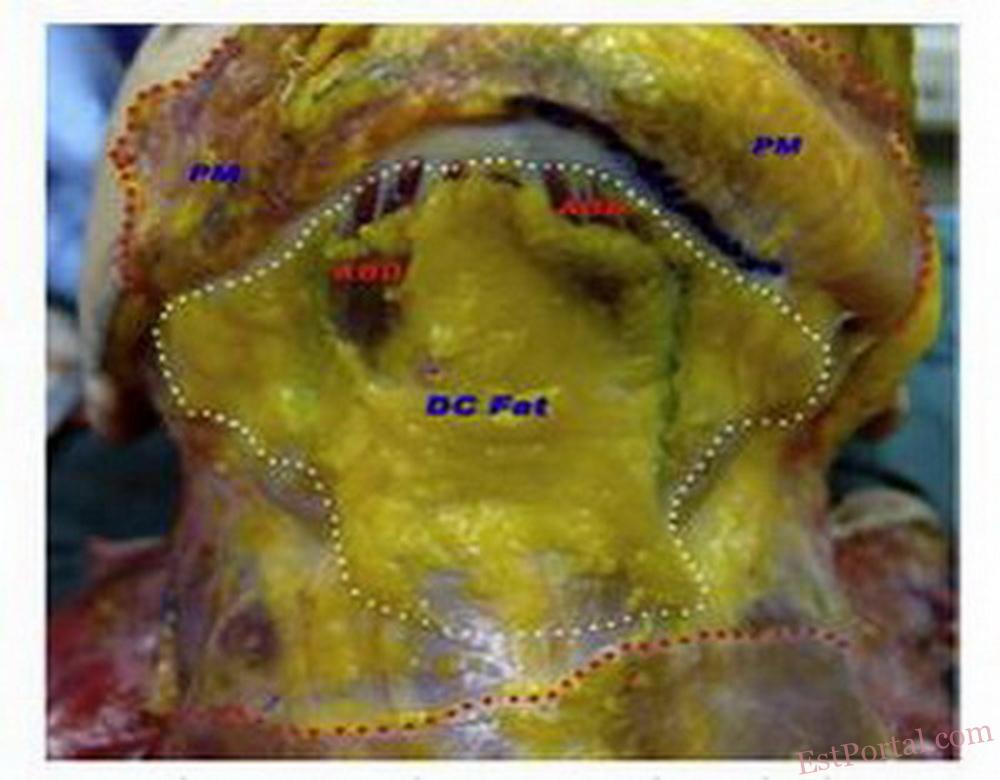
Рис. 8. Эта анатомическая заготовка демонстрирует глубинный отдел шеи. Он имеет типичную трапециевидную форму и проходит на уровне слюнной железы сбоку. Красные пунктирные линии указывают уровень деления мышцы платизмы. Синие пунктирные линии указывают на костные соединения платизменной мышцы. Белые пунктирные линии указывают на грани нахождения глубокого шейного жира. АВD — передняя часть двубрюшной мышцы. DC Fat — глубокий шейный жир. РМ — мышца платизмы, поднятая над нижней челюстью.
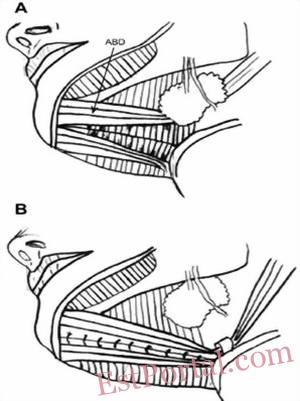
Рис. 9. После резекции шейного жира передняя часть двубрюшной мышцы может быть прошита швами, как корсет, через среднюю линию. А — до двубрюшного корсета. В — после двубрюшного корсета.
Вы можете предсказать высокую вероятность такого исполнения в случае тяжёлой, короткой шеи. После того как поверхностный жир удалён, проводится оценка контура шеи. В случае наличия выпуклостей диссекция проводится по средней линии, открывая платизму, затем применяется поэтапный подход к подплатизменным структурам, начиная с глубокого жира (Рис. 7).
Этот жир не ограничивается только зоной двубрюшной мышцы. Он имеет трапециевидную форму и проходит сбоку в зону под слюнными железами (Рис. 8).11 Если вы удалите только центральную часть, вы получите неровный участок под подбородком.
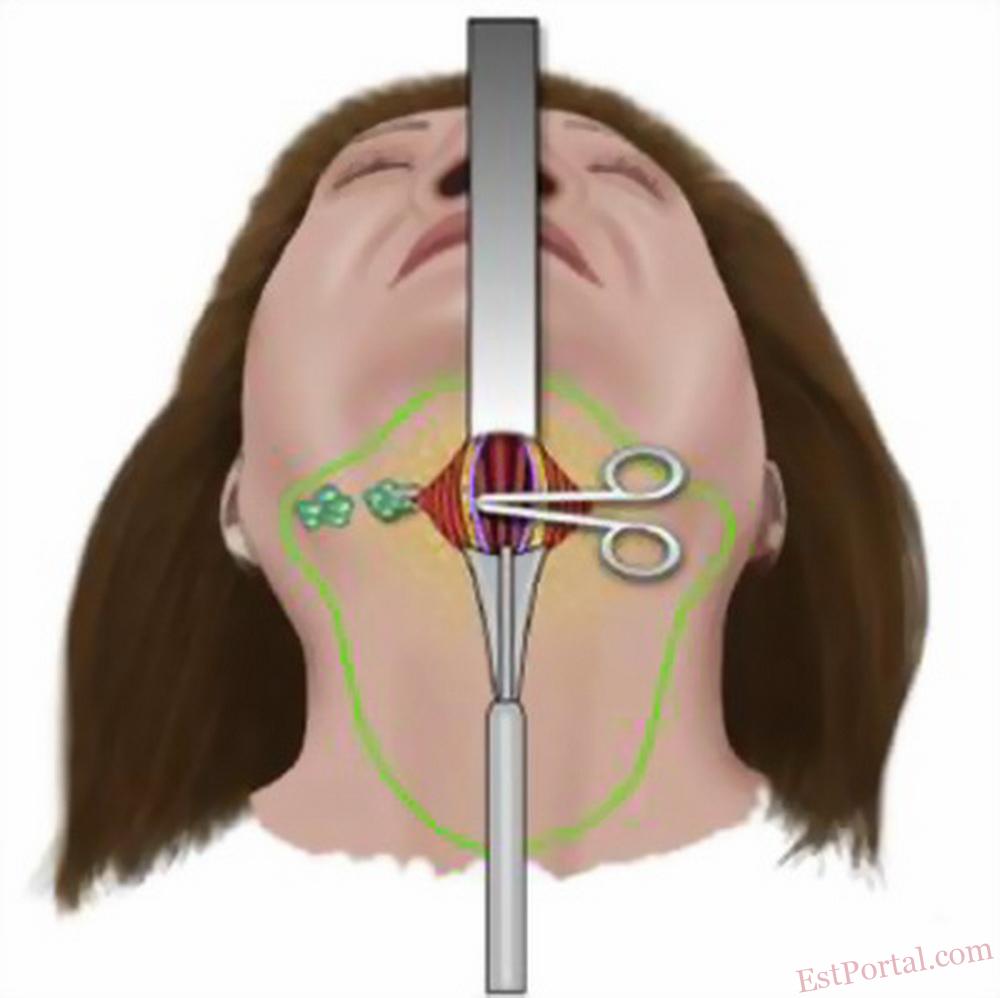
Следующим шагом оценивается контур двубрюшной мышцы напротив челюстно-подъязычной мышцы. Если двубрюшная мышца выпуклая, то первым шагом становится попытка поднять эту мышцу по средней линии. Если она заполнит полость, и контур улучшится, то используем корсет из инвертированных швов 3-0 нейлон для передней части двубрюшной мышцы (Рис. 9). Если это не улучшит контур, то применяется касательное снятие верхнего слоя передней части двубрюшной мышцы. Если до операции обнаружен птоз или увеличение слюнных желез, или во время операции железы выпуклые, то поверхностная часть железы удаляется с каждой стороны (Рис. 10).
Рис. 10. Частичная резекция слюнной железы путём прямого подплатизменного подхода.
Цервикопластика
Для проведения глубокой цервикопластики нам понадобятся длинные и тонкие инструменты. Я обычно использую два облегчённых ретрактора и контролирую кровотечение двумя малыми зажимами.
- Мышца платизмы закрывается после поднятия в средней линии.
- Если платизма тонкая, я не удаляю излишек. Я её сворачиваю или загибаю края, применяя узловые швы.
- В случае выпуклости платизмы я обычно делаю две Z-пластики на передних 4 см мышцы. Я удерживаю избыточную мышечную ткань с помощью поднятия кисетным тканевым швом Рамиреза и/или я делаю резекцию в самой нижней части зоны, в которой проводится диссекция.
- Я оставляю 2 дренажа-бабочки подключёнными к трубкам вакуумного контейнера, по одной с каждой стороны подплатизменной плоскости и по одной с каждой стороны поверхностной плоскости. Я не использую фибриновый клей. Обычно я снимаю дренажи на 5-6-й день, немного позднее, чем обычно требует стандарт операции. Это помогает мне предотвратить возможную серому.
Следуя этим подсказкам, вы можете получить надёжный и отличный результат. (Рис. 11-14).
Рис. 11. Дооперационный вид 55-летней женщины. Она имеет тупой угол между шеей и подбородком с избытком кожи и мышечной ткани платизмы.
Рис. 12. Послеоперационный вид после полного омоложения лица.
Обратите внимание на гладкую, чистую и хорошо выраженную шею и угол между шеей и подбородком. К пациенту был применён подход в обоих направлениях. Был использован платизмальный корсетный тканевый шов Рамиреза.
Рис. 13. Пациент до и после ТЕАМ омоложения лица. Оно включало в себя глубокую подплатизменную цервикопластику с частичным удалением слюнных желёз слева.
Рис. 14. Пациент до и после ТЕАМ омоложения лица. Лечение тупой шеи требовало подплатизменной глубокой цервикопластики с удалением глубокого шейного жира и гениомандибулярного имплантата подбородка Рамиреза.
Последствия и осложнения
Осложнения и последствия при проведении цервикопластики могут колебаться от простой неприятности до значительной проблемы.
- Поражение одной или нескольких ветвей крайнего нерва нижней челюсти может иметь ужасные последствия для пациента. К счастью, это можно вылечить во многих случаях. Восстановление нерва может быть ускоренно электрической мионевральной стимуляцией. Чтобы минимизировать этот риск, старайтесь избегать агрессивной липосакции и монополярного прижигания.
- Острая гематома в закрытой части может стать осложнением, которое будет угрожать жизни пациента. Любая гипертензия должна быть под контролем, а пациенты должны находиться под постоянным наблюдением, особенно в течение первых суток. Во время хирургического вмешательства гомеостаз должен проверяться биполярным или коаксиальным секционным коагулятором. Сосуды большого и среднего размера должны быть зафиксированы швами или гемо-клипсами.
- Подкожные/подтканевые уплотнения, вызванные серомами и гематомами, могут быть устранены серией инъекций разбавленного Триамцинолона. Предотвращение появления сером включает в себя предотвращение гематомы и использование закрытой системы мелких дренажей в течение нескольких дней.
- Неровности контура от накопления остаточного жира могут быть исправлены липосакцией с использованием малых канюль. Также это можно предотвратить, создавая точный контур острыми ножницами.
- Некроз кожи, вызванный курением или чрезмерным натяжением, требует повторной коррекции после заживления участка и смягчения кожи через несколько месяцев. Предотвращение включает в себя предоперационное воздержание от курения и контроль за натяжением кожи в момент закрытия раны.
- Остаточная выпуклость вследствие гипертрофии передней части двубрюшной мышцы и/или птоз слюнной железы нуждаются в повторной глубокой цервикопластике. Во избежание этих проблем требуется хорошая предоперационная оценка и тщательное хирургическое планирование.
- Малые зоны остаточных тяжей платизмы могут быть улучшены инъекциями ботокса, в то время как большие зоны потребуют повторной платизмопластики. Чтобы избежать остаточных тяжей платизмы, необходимо использовать подходящую хирургическую технику.
В целом срок перед любой повторной процедурой должен включать в себя продолжительное ожидание, минимум 6 месяцев, в идеале 12 месяцев. В любом случае, вопрос психологического характера может привести и к более ранним повторениям операции.
Выводы и обобщения
Таким образом, коррекция эстетических и анатомических деформаций шеи вследствие процесса старения является комплексным процессом, планирование и подходы к которому зависят от первичного осмотра. Хирургические техники должны быть адаптированы к проблемам, с которыми вы можете столкнуться.12 В отличие от других частей тела, в этом случае хорошее знание анатомии является обязательным. Хирургия может быть как очень простой, так и высоко техничной. Хирурги должны иметь в своем арсенале различные хирургические техники для обеспечения наилучшего эстетического результата. Глубокая цервикопластика — это не поверхностная цервикоплистика; это совсем другое хирургическое измерение. Глубокая цервикопластика не по силам для обычного хирурга, занимающегося омоложением лица. Вы должны иметь опыт в диагностике проблем шеи, выполнении необходимых хирургических манёвров и уметь эффективно преодолевать острые и отдалённые осложнения.
Литература:
- Owsley JQ Jr. SMAS-platysma facelift. A bidirectional cervicofacial rhytidectomy. Clin Plast Surg 1983; 10(3): 429–40.
- Labbe D, Franco RG, Nicolas J. Platysma suspension and platysmaplasty during neck lift: anatomical study an analysis of 30 cases. Plast Reconstr Surg 2006; 117(6): 2001–7.
- Millard DR Jr, Garst WP, Beck RL, et al. Submental and submandibular lipectomy in conjunction with face lift, in the male or female. Plast Reconstr Surg 1972; 49(4): 385–91.
- Fuente del Campo A. Midline platysma muscular overlap for neck restoration. Plast Reconstr Surg 1998; 102(5): 1710–4.
- Ramirez OM. Cervicoplasty: non-excisional anterior approach. Plast Reconstr Surg 1997; 99: 1576–85.
- Ramirez OM, Robertson KM. Comprehensive approach to rejuvenation of the neck. Facial Plast Surg 2001; 17(2): 129–40.
- Giampapa VC, Bitzos I, Ramirez OM, et al. Suture suspension platysmaplasty for neck rejuvenation revisited: technical fine points for improving outcomes. Aesthetic Plast Surg 2005; 29(5): 341–50.
- Giampapa VC, Bitzos I, Ramirez OM, et al. Longterm results of suture suspension platysmaplasty for neck rejuvenation: a 13-year follow-up evaluation. Aesthetic Plast Surg 2005; 29(5): 332–40.
- Giampapa VC, DiBernardo BE. Neck recontouring with suture suspension and liposuction: an alternative for the early rhytidectomy candidate. Aesthetic Plast Surg 1995; 19(3): 217–23.
- Ramirez OM. Cervicoplasty without skin excision. In: Shiffman MA, Mirrafati SJ, Lam SM, et al, editors. Simplified facial rejuvenation. Berlin: Springer Verlag; p. 613–20 Chapter 80.
- Ramirez OM. Advanced considerations determining procedure selection in cervicoplasty. Part one: anatomy and aesthetics. Clin Plast Surg 2008; 35(4): 679–90.
- Ramirez OM. Advanced considerations determining procedure selection in cervicoplasty. Part two: surgery. Clin Plast Surg 2008; 35(4): 691–709.
Оскар РАМИРЕЗ — доктор медицины, пластический хирург, сертифицированный Американской Коллегией пластической хирургии, входящий в ТОП-3 пластических хирургов мира (США)